
 Remember to bookmark this page so that you can find it later.
Remember to bookmark this page so that you can find it later.If you need help, you can find instructions on how to bookmark/favourite content here
exp date isn't null, but text field is

 Remember to bookmark this page so that you can find it later.
Remember to bookmark this page so that you can find it later.
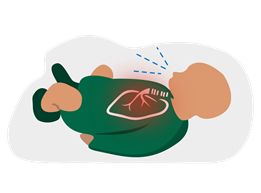
Bronchiolitis is when the smallest air passages in your baby’s lungs become swollen. This can make it harder for your baby to breathe.
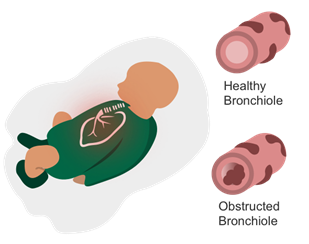
Bronchiolitis is usually caused by a virus called respiratory syncytial virus (known as RSV). Almost all children will have had an infection caused by RSV by the time they are two years old.
RSV is more common in the winter months. Most children will only have mild ‘cold-like’ symptoms and will get better on their own. Some babies can find it hard to breathe or feed and may need to go to hospital.
The virus that causes bronchiolitis in babies also causes coughs and colds in older children and adults, so it is very hard to prevent your child getting it.
Make sure your baby is not exposed to tobacco smoke. Passive smoking can seriously damage your baby’s health. It makes breathing problems like bronchiolitis worse.
If you would like help to give up smoking you can get information / advice from your local pharmacist, GP surgery or by calling the Quit Your Way Scotland helpline on 0800 84 84 84 Mon-Fri 0800-2200 and Sat-Sun 0900-1700.
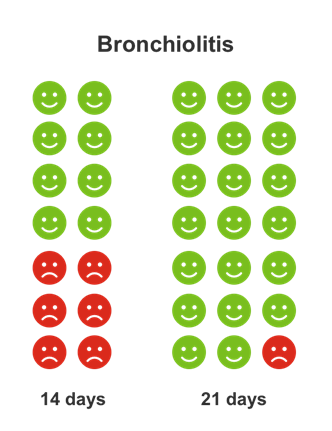
The chart above show how long bronchiolitis lasts in children. The faces represent 10 children who have bronchiolitis. Green faces are those children who have recovered within that time period.
Diagram taken from www.whenshouldiworry.com
Use the table below to know when and where to get help for your child.
 |
|
|---|---|
|
If your child has any of the following signs:
|
You need help now. Go to the nearest Hospital Emergency Department or phone 999 |
 |
|
|---|---|
|
If your child has any of the following signs:
|
You need to speak to a doctor or nurse today. Phone your GP surgery or call NHS 111 - dial 111 |
 |
|
|---|---|
|
If your child has none of the above signs
|
Self care You can keep looking after your child at home. Phone NHS 24- dial 111 if you are concerned. |
Content adapted with permission from the what0-18.nhs.uk resource produced by the Healthier Together initiative

Last reviewed: 09 December 2024
Next review: 31 December 2029
Author(s): Dr Morag Wilson, adapted from Healthier Together
Version: 2
Approved By: RHC Medical Paediatric Governance Group